Beyond clinical diagnosis
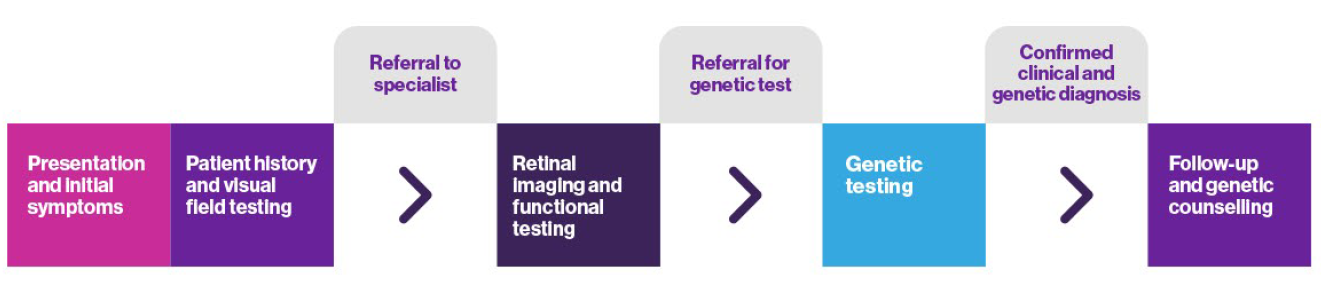
Steps to achieving a full diagnosis in IRD
It looks like you are using an older version of Internet Explorer which is not supported. We advise that you update your browser to the latest version of Microsoft Edge, or consider using other browsers such as Chrome, Firefox or Safari.
Steps to achieving a full diagnosis in IRD
Retinal dystrophies can be categorised in several ways including if they are syndromic (those affecting other organ systems, e.g. Usher syndrome), or non-syndromic (those where the symptoms are solely vision-related) and by the subtype of cell that is predominantly affected.1,2
In conditions where rod cells are more severely affected, night time or low-light and peripheral vision will be affected before degeneration of the central macula and colour vision. In those where cone cells are primarily affected, the primary signs may be photophobia, central visual acuity and reduced colour and contrast sensitivity before further visual impairment becomes apparent.1
This video features a patient and her family discovering the symptoms and diagnosis of IRD. The family shares reasons for pursuing a genetic test and details their life after the diagnosis.
Because of the number of diseases that are included in the term inherited retinal dystrophy, there are a wide range of different signs and symptoms that include loss of night vision, visual field, colour vision, and central acuity.1 Initial symptoms that may indicate a likelihood of an IRD include:

In babies and young children

In older children, teenagers and adults
Beyond standard visual field testing and retinal imaging, there are a number of testing options available to help confirm diagnosis of a specific IRD.1 Some of the more commonly used examples are outlined below.
Using a skin electrode in young children or contact lens electrodes with older children and adults.
Flash, pattern, and flicker light stimuli are used to detect photoreceptor response and function.1

Lipofuscin, a fluorophore, is stored in the retinal pigment epithelium and can act as a surrogate marker of photoreceptor activity that can be picked up by fundus autofluorescence. Different patterns of fluorescence can indicate particular diagnoses.1

OCT uses light reflection to visualise the structure of different layers of the retina in fine detail. It can be used to measure retinal thickening and to determine the level of progression of retinal dystrophies.1

Previously, diagnosis of IRD has relied heavily on clinical testing. This is partly due to the accessibility of genetic testing, but also the availability of clinical trials and approved therapies requiring a genetic diagnosis. With the development of new screening methods and with new research into treatments for specific gene mutations it is now more important for patients to receive a genetic diagnosis.
Deciding if your patient meets the criteria for genetic testing
Genetic testing is appropriate for most patients with presumed genetically caused retinal degeneration. Consider testing if:
Patient meets criteria for suspected IRD5
Patient displays symptoms including :

Has a diagnosis of an inherited retinal dystrophy, or a family history of IRD5
Once your patient is suspected of having an IRD, consider ordering a genetic test.
Genetic testing provides more information about your patient's IRD and is the only way of confirming which genes are affected. It refines the diagnosis and prognosis, allows for better disease management and can identify or confirm eligibility for natural history studies of clinical trials.5 Patients may benefit from access to a genetic counsellor when receiving a genetic diagnosis. The process for ordering a genetic test can differ from laboratory to laboratory, so please check with the relevant centre in your country (see below).
Where to refer a patient
You can refer your patient to centres for genetic testing within your country.
_________________
